ICU with a View

Traditionally, intensive care units have been intimidating institutional spaces with long, cloistered hallways, fluorescent lights, and small patient rooms jam-packed with monitors and machines.
Patients were often in bed for the duration of their stay. Visitors were limited to specific hours and, even then, often one at a time. The environment was decidedly not warm and welcoming.
But times have changed. And just as critical care medicine has evolved, health care architects and medical planners are designing ICUs differently as well, taking a person-centered approach and applying evidence-based design.
ICU patients, for example, have benefited from research showing that exposure to natural light cycles (day/night) lessens ICU delirium. A family area in patient rooms allows for caretaker support, vital to patient healing. And views of nature and greenery lower anxiety in patients, visitors, and staff.
Craig Jabaley, associate director of the Emory Critical Care Center and associate professor of anesthesiology, has worked with the Society of Critical Care Medicine on ICU design guidelines.
“There has been a shift from an illness-centered environment to one focused on ‘ICU liberation,’” which means getting folks through their critical illness to recovery, back to being contributing members of society,” says Jabaley.
“Historically, we were doing a good job of keeping people alive, sustaining organ function. But we were not doing as good a job in other areas such as preventing delirium, encouraging early mobility, and family engagement and empowerment.”
As these shifts occurred in critical care medicine, ICU design evolved to support the changes.
We spoke with several Emory Healthcare staff, from nurses to doctors to advanced prac- tice providers who work in ICUs and have been involved in the planning, design, or remodeling of an intensive care unit recently.
The following are their thoughts on advances in ICU design.
MANY VOICES
An overwhelmingly positive advance, all agree, is that multiple stakeholders have been invited into the modern planning process, from ICU staff to patient advisers.
“The most important need from a physician standpoint,” says intensivist Michael Waldman, critical care specialist at Emory Healthcare, “is the ability to have more tech in the ICU and more advanced monitoring systems—basically, an ICU built to take on advances in care.”
Nurses echo that sentiment, saying that not only more space but thoughtful room layout is vital. “We’ve had to design for the changes in how we care for patients and for a tremendous number of new technologies,” says Toni Ash, a nurse with Emory Healthcare for four decades and unit director of a cardiovascular surgical ICU.
Ash recalls visiting a “cardboard city” model unit and room and the feedback from staff: “What is the best way to maneuver around the bed? If the doctor needs to intubate, do they come in from the right or left? We talked through every detail for hours.”
Clinical nurse specialist Mary Still says her team talked through the physical structure of patient rooms, how the monitor and all the equipment would flow together, the patient’s position, and the ability to turn the patient’s bed.
“We actually put someone in the bed and moved them around to see how it worked,” she says.
What most hospitals have found is that the more tech-laden ICUs have become, the more flexibility is provided by an articulated ceiling-mounted boom when possible.
“We do a lot of procedures in ICU patient rooms, so we wanted to get rid of the pain points we were having in our older ICUs and make sure it was easy and safe to do these procedures,”
says Dave Carpenter, physician assistant and codirector for quality and patient safety for the Emory Critical Care Center. “That means being able to get around the bed, good lighting, no tubes to trip over. In the new rooms, the way the booms are arranged, you can walk behind the bed quite easily.”
FAMILY CARE
Family and patient reps expressed a desire for comfortable sleeping areas and private bathrooms as well as places to work, study, or watch TV so they can “still carry on with part of their normal life,” says Still.
“Our older units had zero places for families. They were smaller rooms with just enough space for the patient and a nurse,” says Missy Anderson, assistant nurse manager of a cardiovascular surgical ICU.
“Now, families are welcomed in; there is a space for them to call their own. They are asked to participate in rounds, in conversations . . . there aren’t locked doors or us saying ‘No, you can’t come in right now.’"
“It means a lot to families to have their own space, a sofa that pulls out into a twin bed, capability to plug in their phones and computers, storage under the bed and in family lockers on the unit,” adds Stephanie Pieroni, unit nursing director of a surgical transplant ICU. “We put an extra chair in the room so a physician/provider could sit down and talk to family members eye to eye, for more of a connection. And most of the unit has a great view of the city through big picture windows.”
Staff appreciate the windows as well, she says. “Especially in the winter, you might come in to work when it’s dark and leave after it’s dark. It’s nice to see the change of scenery and light during the day.”
PATIENT ACUITY
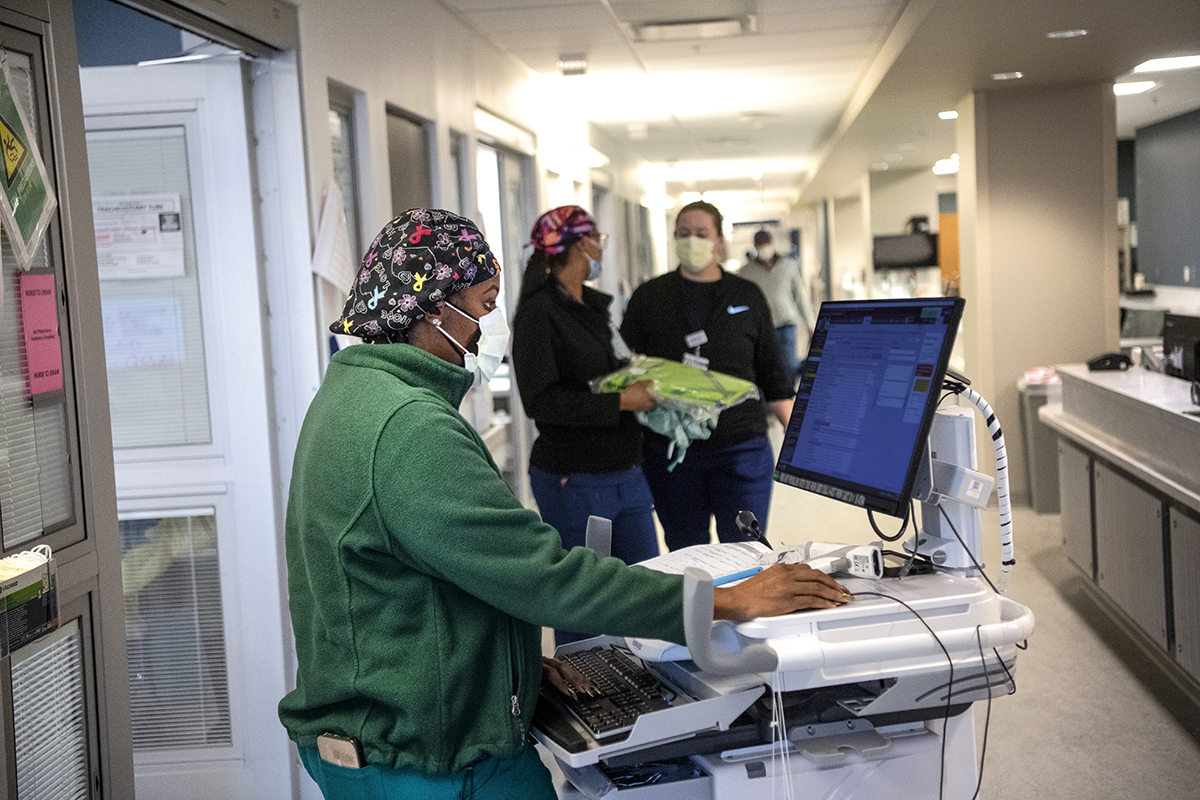
“Nurses stations have a line of sight directly into patient rooms,” says Still. “They can observe the patient, see interactions with providers, and can tell when a crisis is going on. That enhances everyone’s comfort.“
Monitors are placed throughout the unit so vital signs are visible to all nurses taking care of patients. Personal protective equipment (PPE) closets are often just outside the rooms, stocked with gowns, gloves, masks, etc.
“We purposely did not put a nook or sitting area between patient rooms,” says Pieroni. “Now we can pair patients according to acuity and still have the line of sight we need to be able to care for them safely.”
Having ICU rooms all on one floor is helpful, says Rose White, ICU nursing unit director at Emory Hillandale Hospital, not only for patient safety but for staffing as well.
“Two different floors were hard to juggle,” she says. “One floor will allow a lot more efficiency. And we love having glass doors to the rooms, so we can see the patients at all times.”
COLLABORATION SPACE
The ICU is a more collaborative environment now, with intensive–care trained physicians, intensive–care trained advanced practice providers (APPs), highly subspecialized nurses for each type of ICU, respiratory therapists, pharmacists, nutrition support specialists, patient care technicians, social workers, and “an army of consultants.”
ICUs, then, must be designed in ways that facilitate this collaboration, with more open space, seating, computers, and areas for charting, teaching, and conversation.
Separate rooms for medical students, residents, APPs, and family conferences right on the unit also are essential, as are break rooms and water stations.
Newer Emory Healthcare ICUs have included “relaxation rooms” with massage chairs for staff and access to an outside garden or roof terrace.
A few human touches nearly everyone mentions are dimmers for the lights at night to synch with patients’ circadian rhythms and keeping the unit as quiet as possible during sleep hours.
Finding a place for all the machinery and accessories needed in critical care remains a challenge, but many ICUs are leaning toward large, undefined storage spaces and creative storage solutions in patient rooms.
“We actually engage process engineers to help us figure out how to shoehorn all the things we need into the space we have,” says Jabaley. “I want the units to be flexible enough to accommodate patients and technologies 20 years into the future.”
Email the Editor