A Life Consumed by Sleep

Nothing he had tried had worked. For Sigurjon Jakobsson, the overseas trip was a last-ditch effort to seek out a treatment that would help him wake up. He had struggled with sleeping excessively for several years before traveling from Iceland to Atlanta to see a visionary neurologist who might have some answers.
In high school, Sigurjon was a young decathlete, competing as part of Iceland’s national sports team. But at the age of 16, an increasing need for sleep began to encroach upon his life. Sigurjon needed several alarm clocks to get out of bed and was frequently late to school or his job at a construction company. He often slept more than 16 hours a day.
When Sigurjon describes his experiences, they sound like depression, although his mood and lack of motivation appear more a consequence of his insatiable desire to sleep than a cause. He quit sports. He dropped out of college, became isolated, and lost touch with close friends.
“Your will to do things just kind of dies,” he says. “And then you’re always trying and trying again. It just gets worse. You kind of die inside from being tired all the time.”
At the recommendation of a neurologist in Iceland, Sigurjon’s family sought out Emory Brain Health Center’s David Rye, who is known internationally for his research on idiopathic hypersomnia, a poorly understood sleep disorder.
Sigurjon’s profile suggested that he might respond to an unconventional medication Rye has experience with: flumazenil. It was not originally developed for use with sleep disorders and is generally given intravenously. It is available in an oral lozenge form, and a cream applied to the skin, through only a few compounding pharmacies in the U.S.
Sigurjon Jakobsson traveled from Iceland to Atlanta with his parents for treatment for his hypersomnia. 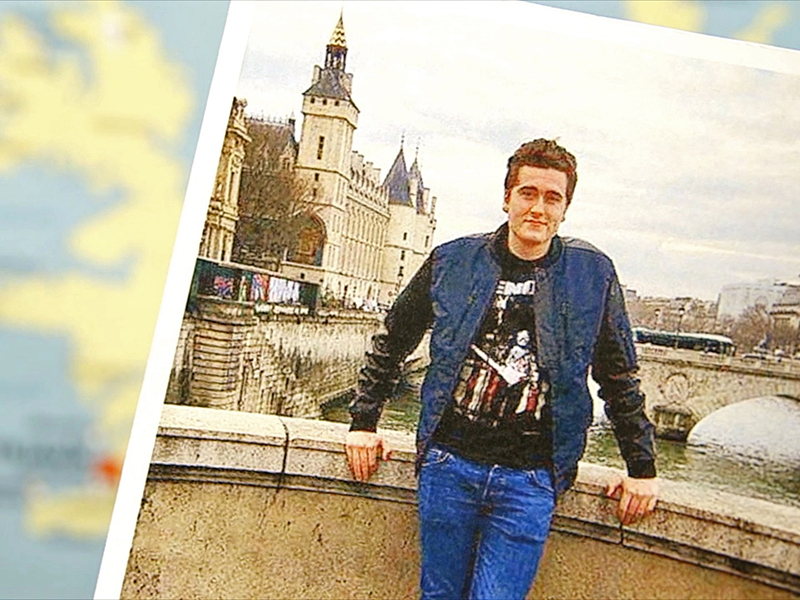
After evaluating Sigurjon’s medical history and symptoms and giving him a series of tests, Rye concluded that he has idiopathic hypersomnia.
“When you listen to him,” Rye says, “he sleeps too much, he has a hard time waking up, he takes long naps, he has ‘sleep drunkenness’ . . . that’s hypersomnia.”
For several years, Rye has been calling attention to the neglected status of idiopathic hypersomnia. Hypersomnia means “too much sleep,” but the word idiopathic can be confounding. It means the cause is not known.
Sleep scientists have argued about IH’s origin and mechanisms and whether it’s one, two, or many entities. Rye and his team have an idea for how to redraw the map. “We’re trying to change sleep medicine here,” Rye says. “We want to at least get patients in through the right doorway so that we can direct them more swiftly to an accurate diagnosis and a tailored treatment.”
Sleep specialists are trained to recognize conditions that can render someone drowsy, with two of the most common being sleep apnea and narcolepsy.
Sleep apnea comes from interruptions in breathing, which interfere with sleep’s restorative nature and put strain on the heart.
Narcolepsy is a sleep disorder characterized by excessive sleepiness, sleep paralysis, hallucinations, and in some cases episodes of cataplexy—partial or total loss of muscle control, often triggered by a strong emotion such as laughter. One form of narcolepsy occurs when an autoimmune attack eliminates cells in the brain that keep someone awake and alert.
But some people with persistent sleepiness don’t fit neatly into either of these categories. Understanding what lies behind their sleepiness could unlock new insights into how the brain works. It could also change the lives of people, such as Sigurjon, who have slipped through the cracks of modern medicine.
Rye compares hypersomnia and narcolepsy to “apples and oranges.” He has proposed that in some people with symptoms like Sigurjon’s, the circuits within the brain that promote and maintain sleep are overactive. This idea is supported by the Emory team’s use of flumazenil for hypersomnia and similar disorders.
Flumazenil is an antidote against benzodiazepines and related compounds—a class of anti-anxiety and sedative drugs, such as alprazolam (Xanax), zolpidem (Ambien), diazepam (Valium), and midazolam (Versed). People undergoing an uncomfortable medical procedure, such as a colonoscopy, are often given Versed for “conscious sedation.” If they get too much and have trouble breathing, flumazenil can reverse the sedation. It can also be used to counteract overdoses of benzodiazepines in the ER.
In 2007, Rye and his colleagues observed flumazenil’s effects with Anna Sumner Pieschel, an Atlanta attorney whose life was being overtaken by sleep. Due to hypersomnia, Anna had to take a leave from her job and couldn’t drive. She had tried conventional medications, such as the “smart drug” modafinil, together with amphetamines, but found it difficult to tolerate the doses she needed to stay awake and experienced periodic crashes.
Rye has compared Anna’s treatment with stimulants to “driving a car with the parking brake on.” He and a colleague, nurse practitioner and former Emory sleep researcher Kathy Parker, suspected something else was going on. Laboratory tests indicated that Anna’s spinal fluid mimicked the effects of benzodiazepines, even though she wasn’t taking any.
Looking for alternatives, Rye and Parker obtained flumazenil from manufacturer Hoffmann-La Roche through a limited “compassionate use” arrangement. They figured out how to deliver it as under-the-tongue lozenges and a skin cream. Flumazenil—in combination with other medications—helped Anna return to work. She eventually became a partner at her firm, got married, and started a family.
Nodding toward her energetic preschool-aged son, Anna says: “If you told me six years ago that this would be my life, I wouldn’t have thought it was possible… Today I have everything I never thought I would have.”
Likewise, Sigurjon’s family, and some of the doctors he saw in Iceland, were unsure how to help him. He had already tried other medications that are often used to treat persistent sleepiness: modafinil and methylphenidate (Ritalin). They could physically keep him awake, but he still didn’t feel right.
David Rye, professor of neurology and director of research for Emory Healthcare's Program in Sleep Medicine; Andrew Jenkins, associate professor of anesthesiology; and Anna Sumner Pieschel, an Atlanta attorney successfully treated for hypersomnia. 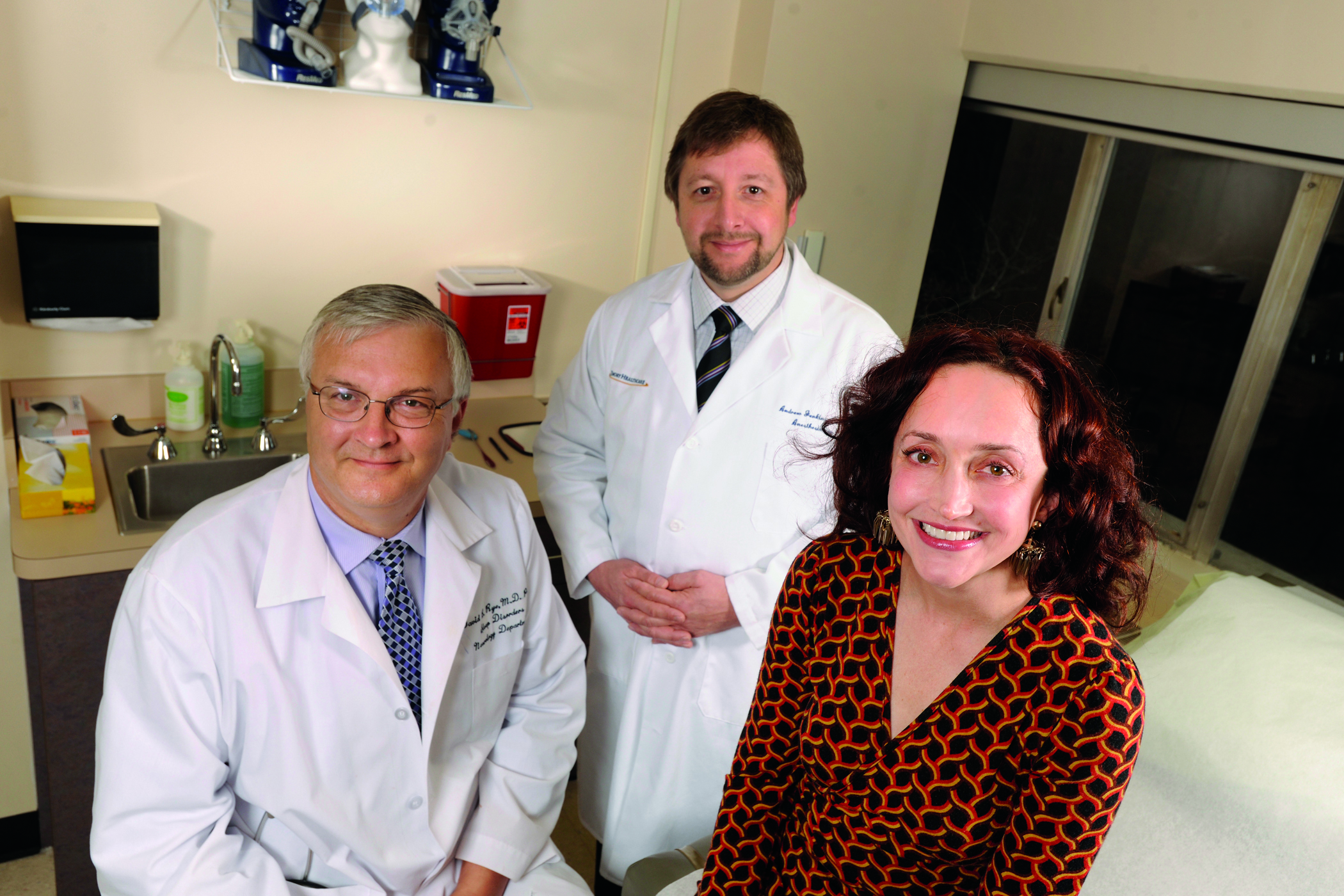
In July 2018, Sigurjon, then 23, came to Atlanta to see Rye and got a chance to let a flumazenil lozenge dissolve under his tongue. As seen in a Georgia Public Broadcasting video filmed for the Emory/GPB series Your Fantastic Mind, both his family and Anna were watching. The effect was not immediate. “This is my last resort,” he said. “If this doesn’t work, I don’t know.”
Sigurjon first felt agitation in his legs: “My body is telling me to go move…to go running or go do something.” Within five minutes the drug’s effects began to kick in and he smiled. “It’s like my eyes are being lifted up and yeah—it’s a strange feeling,” he said. “It feels really good…I don’t even remember feeling like this.” The Emory researchers monitored physical changes in his alertness, with an EEG, to rule out the placebo effect. On days he tried flumazenil, he performed tests measuring his reaction time, which became faster after taking the drug. In addition, after applying a skin cream containing flumazenil, he was able to wake up spontaneously for the first time in years —to his surprise—without the aid of an alarm clock.
In January 2019, Sigurjon told Rye he was slowly building stamina to be able to work at his construction job and perhaps return to school. Rye has other patients from European countries who periodically visit Atlanta for check-ups and to maintain their flumazenil prescriptions.
Flumazenil is not magic, and its effects on healthy or sleep-deprived people have been inconsistent in previous studies.
In a review of 153 Emory Sleep Center patients who didn’t respond well to conventional stimulants, about 60 percent reported that flumazenil helped them become more awake. A smaller number (39 percent) stuck with the drug long term; the effects weakened over time in a few patients. The most common side effects were dizziness and anxiety. Still, the drug offers hope to people with hypersomnia who have had to stop school, leave their jobs, or apply for disability.
A recently formed nonprofit, the Hypersomnia Foundation, is working to raise awareness and promote research. It hosts an annual conference—the first of which was held at Emory. Rye chairs its scientific advisory board and Lynn Marie Trotti, Emory associate professor of neurology and sleep specialist, chairs its medical advisory board. “For some people, hypersomnia really puts their lives on hold, especially if the usual medications don’t work for them,” Trotti says. “We’re seeking a better understanding of the disorder.”





