Working to Cure What Ails You

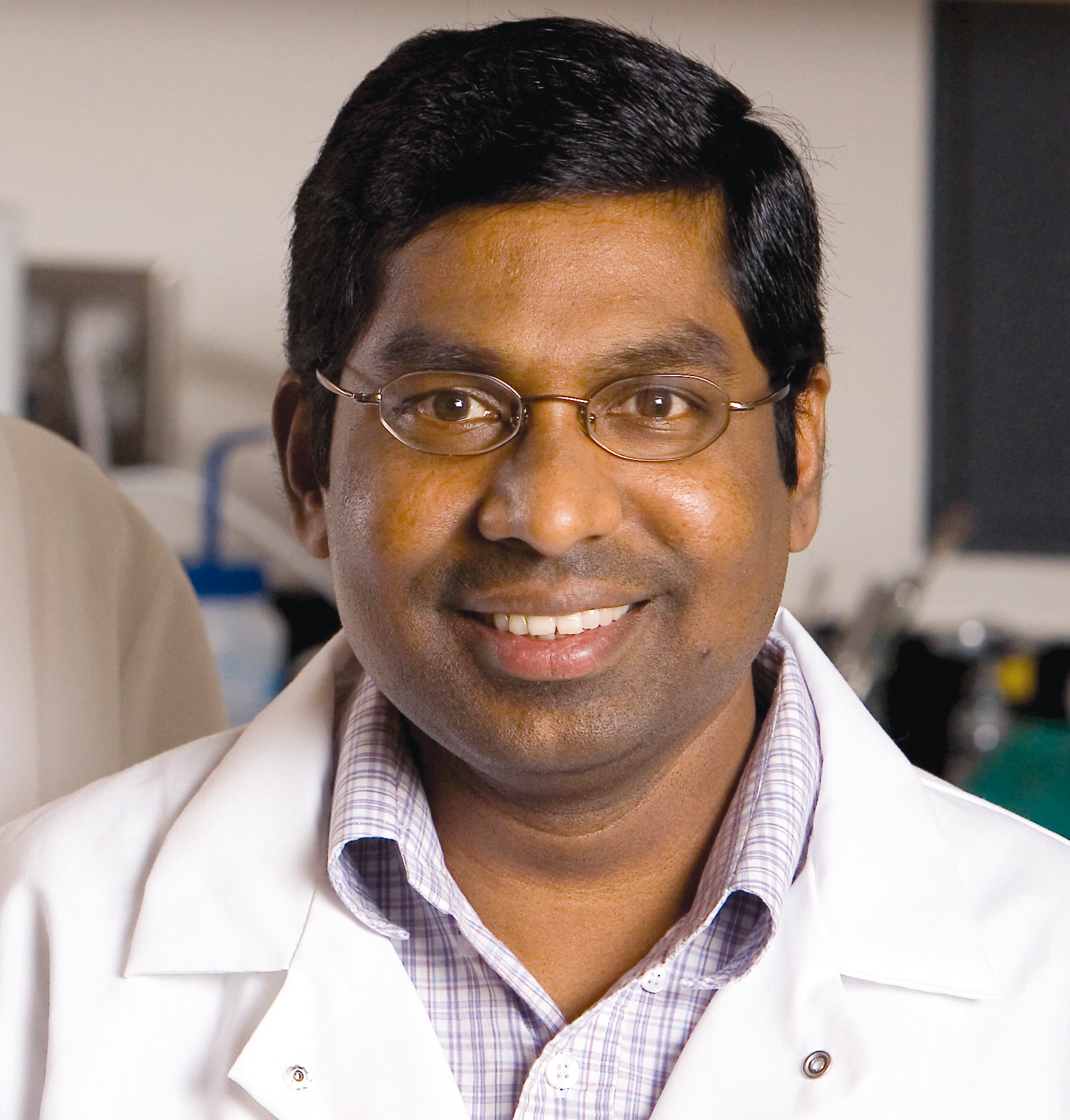
Yerkes Director R. Paul Johnson
Promising HIV/AIDS vaccines. A test to predict Alzheimer's. Novel treatments for autism. A deeper understanding of social status and its impact on health. Improved anti-rejection drugs for organ recipients. And the list goes on.

R. Paul Johnson, Yerkes director, whose own research centers on HIV and immunity.
As one of seven nonhuman primate research centers in the country, Emory's Yerkes National Primate Research Center brings together a diverse group of scientists—from neuroscientists to immunologists—to work on causes, preventions, treatments, and cures for a host of human diseases. Yerkes researchers also conduct studies to glean a greater understanding of evolution and how humans are linked to their primate cousins.
Established in 1930 by primatologist Robert Yerkes, the center now has more than 3,000 primates, including rhesus macaques, sooty mangabeys, and cynomolgus monkeys, as well as a vivarium with 7,500 rodents, including mice, rats, and voles.
On the following pages, we take a look at the most transformative discoveries and life-saving treatments to have emerged from Yerkes.
HIV/AIDS: Prime Time

HIV has become a life sentence instead of a death sentence, but a vaccine remains out of reach.
"I certainly believe an HIV vaccine is achievable," says microbiologist and immunologist Rama Amara. "We've already made remarkable gains, and this would not have been possible without everything we've learned through our work with the monkeys."
Amara has just received National Institute of Health (NIH) funding to take a vaccine he developed through the first phase of a clinical trial to test its safety. This vaccine builds upon the work of Harriet Robinson, who pioneered a DNA-based vaccine that stimulates an immune response by using only pieces of the virus instead of the virus itself, so the recipient is never placed at risk of infection.
Robinson's original vaccine regimen consists of two inoculations of noninfectious HIV particles to prime the immune response, followed by two inoculations of a weakened smallpox vaccine to boost that response.
The vaccine was effective in preventing the spread of SIV (the monkey version of HIV) in some of the vaccinated animals. Robinson, now an emeritus professor of microbiology and immunology at Emory School of Medicine, is continuing work on vaccines for HIV, Zika, and other human viruses at the biomedical company GeoVax, where she is chief scientific officer.
Amara's vaccine includes the addition of a protein—CD40 ligand—which was shown to improve protection in monkeys.
Amara's colleague, Cynthia Derdeyn, uses studies of human subjects and nonhuman primate models to develop novel antibody-based vaccination strategies for HIV. Highlights of her recent work include tracking exactly how the crafty virus evades obstacles posed by the immune system. "The goal is to generate antibodies that can attack the virus particle as well as virus-infected cells," says Derdeyn.
A vaccine will come too late for the millions already infected with HIV, so Yerkes researchers are also working to find a cure. HIV is hard to get rid of for many reasons, but one is that even when it is suppressed by antiretroviral drugs, a bit of the virus hides out in reservoirs in special areas of the lymph nodes. Georgia Research Alliance Eminent Scholar Guido Silvestri and colleague Mirko Paiardini are leading studies to find ways to kick the virus out of its hiding places and then kill it with a vaccine and/or drugs.
Autism: Chemical Bonds

Call it "vole love."
Larry Young has been trying to discover what makes humans able to establish relationships by studying two species of these small rodents.
Prairie voles are monogamous, forming bonds that last their entire short lives. Their close cousins, meadow voles, are promiscuous.
Through decades of research, Young has been able to tease out the brain chemistry and circuity that underlies the prairie voles' ability to form and maintain relationships.
Because relationships are not easy for people with autism, Young thinks his discoveries may lead to better understanding and treatments for the disorder. "In people with autism, social information does not activate the reward center of the brain as it does for the rest of us, so in their minds, social information is no more important than any other type of information," Young says.
This makes it hard for them to infer emotion, remember faces, feel empathy—things that are necessary to form strong social bonds.
"We know the brain chemistry and circuitry behind these abilities," he says, "so now we are trying to find ways to tweak the system in those with autism."
Some of the more promising work revolves around the hormone oxytocin (not to be confused with the synthetic opiate oxycontin), which is the magic ingredient behind the strong maternal bond as well as the glue between lovers. It also sharpens the brain's attention to social cues. Prairie voles' brain reward centers are highly sensitive to oxytocin—their meadow cousins, not so much.
If you could boost oxytocin uptake in those with autism, they might become more aware of social cues. The problem is that only a tiny amount of synthetic oxytocin is able to make it past the blood-brain barrier into the brain.
Young has found a new drug that stimulates the natural release of oxytocin in voles, inducing them to form a pair bond even without mating. He is testing it in humans in an Australian clinical trial. "I don't think giving a child oxytocin and sending him off to school would be the best approach," says Young. "A person who has autism is likely to get as many negative social cues in a day as he does positive ones. Making him more attentive to those could be damaging."
However, says Young, boosting social learning in therapy could make the sessions more productive.
Oxytocin is just one of the avenues he is pursuing with voles: "By understanding the neurochemistry involved in social engagement, we hope to find novel ideas for improving social functioning in those with social deficits."
Antirejection drugs: Transplant Solutions
Sometimes, the cure can be nearly as problematic as the cause.
Until six years ago, the best drugs available to prevent organ rejection after a kidney transplant were members of the cyclosporine family (CNIs)—which are actually toxic to the kidney. The drugs, which must be taken for the rest of a patient's life,
also trigger a host of ills, including high blood pressure, elevated cholesterol, and diabetes. On average, a kidney recipient on cyclosporine can expect to live eight to 10 years after the transplant without another transplant.
The game changed in 2011, when the Food and Drug Administration approved belatacept, which, unlike CNIs, selectively targets the immune system and prevents rejection without damaging the kidneys or increasing cardiovascular risk.
FDA approval was the finish line of a journey that began in the 1990s at Emory and Yerkes. Transplant surgeons Christian Larsen and Thomas Pearson worked first with rats and then with monkeys on development of the breakthrough drug. "In our clinical practice we saw how transplantation could transform lives, but at the same time we saw how the very drugs that we were using to prevent rejection ultimately caused the transplants to fail prematurely," says Larsen. "We were extremely fortunate to be undertaking our studies at Emory, where we could move seamlessly from the lab to Yerkes and then to clinical trials, saving years in the development program."
Belatacept has not yet deposed CNIs as the gold standard for kidney transplant patients. About 3,000 people in the U.S., including nearly 1,000 at Emory, are on the drug. That is likely to change after a report in the New England Journal of Medicine showed that seven years after transplant surgery, patients on belatacept were 43% less likely to die of organ rejection than those who took cyclosporine. And the kidneys of the belatacept patients functioned as well in year seven as they did in year one.
"This is a really big step toward having one transplant last for a lifetime, which has been sadly far from the case for the majority of people," says Larsen. "We've got work to do but belatacept also holds promise for use in transplants of other organs, such as hearts and lungs."
Social intelligence: Share and Share Alike
Empathy, fairness, and a sense of morality have long been considered uniquely human traits.
Then primatologist Frans de Waal shook perceptions with his research uncovering similar attributes in monkeys and apes. De Waal spent his career studying behavior and social intelligence in primates.
When de Waal first began doing research in the 1970s, ascribing human characteristics such as intentions or emotions to animals was akin to blasphemy. But early on the young scientist observed chimps reconciling and offering comfort after fights, and he became convinced monkeys, apes, and humans shared the ability to understand and respond to others' feelings.
De Waal devoted his career to uncovering the "humanity" in monkeys and apes. His most famous study—an experiment demonstrating that monkeys possess a sense of fairness—came about by accident.
"At that time, scientists considered a sense of fairness a moral principle derived through reasoning and logic," he says. "Because I was studying emotional intelligence, not cognitive intelligence, I was not looking at fairness. My experiment was investigating cooperation in capuchin monkeys."
During the course of that study, however, de Waal noticed that the monkeys paid keen attention to the reward the other monkey was getting.
"If everyone got the same reward for a certain task, they were fine with that and would keep doing the task," he says. "But if one monkey noticed the other one got something better than he did—for example, a grape instead of a cucumber—he would stop doing the task and become upset."
Together with Sarah Brosnan, now a professor at Georgia State University, de Waal replicated the study several times and discovered that chimpanzees took it a step further. When given a choice between getting most of the treats for themselves, or dividing them equally with another chimp, they most often chose the latter.
"We have now reached the point that if you asked me what is the difference between the sense of fairness in humans and in chimpanzees, I would have to say not much," says de Waal. (Yerkes is evaluating donation opportunities for its chimpanzees after the great apes were granted protection under the Endangered Species Act and the NIH moved away from funding behavioral research with them.)
Immune system: Rich Monkey, Poor Monkey

The richest Americans can expect to live more than a decade longer than the poorest.
It's not hard to point the blame—the poor lack adequate access to health care, they are more prone to obesity and tobacco use, and they tend to live in areas more affected by violence and illicit drug use. But it turns out, even if you can factor out all those negatives, poor people may still have a shorter life expectancy. That's because the stress of living on the low rungs of the social ladder sabotages the immune system.
The good news, according to research done at Yerkes in collaboration with Duke and the University of Montreal, is the damage does not have to be permanent. Moving up a rung or two on the social ladder can improve immune function.
Mark Wilson and colleagues discovered the regenerative power of improved social standing by studying female rhesus monkeys, which live in groups organized by a strict social hierarchy both in the wild and in their captive groups at the Yerkes field station in Lawrenceville.
The dominant females have a life of privilege—eating when they want, sitting wherever they want, getting frequent grooming, and picking on subordinates whenever the mood strikes. Females with low rank, on the other hand, eat when the feeding station is available, give up their spot if a dominant female wants it, go without grooming, and endure constant harassment.
"Life can be hard on the lowest rungs of the ladder," says Wilson. "Our data show that these monkeys experience chronic unresolved psychosocial stress. We wanted to look at the consequences of that stress and at possible interventions."
Wilson and the team put unrelated females that didn't know each other into new social groups, introducing them one by one. The females quickly established a pecking order based on seniority.
The researchers then looked at the monkeys' blood. They found genes within immune cells were turned on or off depending on the female's rank, especially within specific types of white blood cells that act as the first line of defense against infection.
In low-ranking monkeys, genes were expressed in a way that caused the white blood cells to go haywire, overexciting the immune system and leading to chronic inflammation which, in turn, left the animals more vulnerable to infection and disease. The genes in high-ranking females, by contrast, were expressed in a way that boosted immune response.
Then, like an episode of Survivor, the monkeys were sorted into new groups and had to establish new hierarchies. Positions changed. Some formerly dominant monkeys were now low in social standing and others moved up the ranks. Remarkably, the monkeys' immune cell regulation changed according to their new rank. Immune response improved in monkeys who rose in social standing and decreased in those who fell.
"This shows that we need to move beyond looking for pharmaceutical solutions to treating the harmful effects of chronic stress," Wilson says. "We need to give people the resources necessary to either remove the stress from their lives or to develop coping strategies to deal with it."
Genes: Monkeying around with genes
Huntington's disease has been likened to having Alzheimer's, Parkinson's, and ALS all at the same time.
Scientists know the cause—a mutation in a single gene—but have not been able to come up with a treatment or cure.
Rodent models of Huntington's, as well as other neurodegenerative disorders, have not proven to be very helpful—rodents with Huntington's don't develop all the same physical symptoms and their cognitive decline and mood swings can be hard to gauge. In a major breakthrough, Anthony Chan developed the first transgenic monkey model of Huntington's. Transgenic animals have a foreign gene deliberately inserted into their genome. Chan's research team at Yerkes injected the mutant gene responsible for Huntington's into mature eggs collected from rhesus macaques. The team then fertilized the eggs in the lab and implanted the embryos into surrogate monkeys.
Chan has followed these monkeys with Huntington's from birth to 10 years, and found that they developed symptoms similar to humans with the disease.
Between 2 and 5 years of age, the monkeys exhibited increasing symptoms of Huntington's. MRI scans also revealed changes in their brains similar to those in humans. Now, his team is expanding the colony with the aim of testing different treatments.
"The work we do with these monkeys will be very translatable to humans," says Chan. "These monkeys will now allow us to evaluate new treatments, such as gene therapy, faster and get them to patients sooner."
Who's Who
Rama Amara and Harriet Robinson
developed an AIDS vaccine now in human trials.
Anthony Chan
created the first transgenic monkey model of Huntington’s disease.
Frans deWaal
has advanced the understanding of emotions such as empathy and altruism.

Larry Young
illuminated the brain chemistry of social relationships and bonding by studying voles.
Chris Larsen and Thomas Pearson
codeveloped a new immunosuppresent, be-latacept, for transplant patients. The drug prevents rejection without damaging the kidneys or increasing cardiovascular risk.
Cynthia Derdeyn
develops novel antibody-based vaccination strategies for HIV.

Mark Wilson
discovered the regenerative power of improved social standing.

To support
Yerkes researchers who are improving human health and lives worldwide, contact Vicki Riedel at 404.778.5939 or vriedel@emory.edu



